- In-Stock Tumor Cell Lines
- Human Orbital Fibroblasts
- Human Microglia
- Human Pulmonary Alveolar Epithelial Cells
- Human Colonic Fibroblasts
- Human Type II Alveolar Epithelial Cells
- Human Valvular Interstitial Cells
- Human Thyroid Epithelial Cells
- C57BL/6 Mouse Dermal Fibroblasts
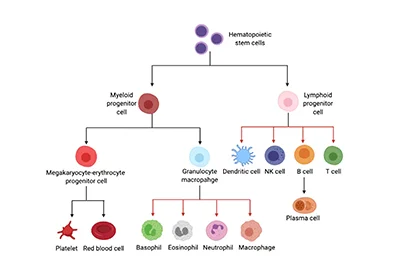
- Human Alveolar Macrophages
- Human Dermal Fibroblasts, Adult
- Human Lung Fibroblasts, Adult
- Human Retinal Muller Cells
- Human Articular Chondrocytes
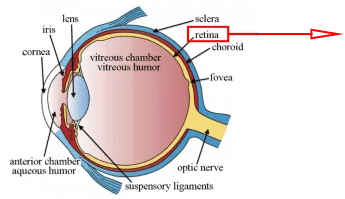
- Human Retinal Pigment Epithelial Cells
- Human Pancreatic Islets of Langerhans Cells
- Human Kidney Podocyte Cells
- Human Renal Proximal Tubule Cells
Eating and drinking may seem simple and routine to us, however, these daily actions constantly challenge the mouth. They expose our mouths to microbes and allergens from outside world, and to micro-injuries from biting and chewing on a daily basis. Thanks to the oral mucosa which is the protective mucous membrane lining the inside of the mouth, the oral cavity is extraordinary efficient at warding off pathogens and healing wounds, thus allows us to live without the constant threat of infections and diseases. So far, scientists still don’t fully understand the mechanism that makes the oral mucosa so resilient. It is important to understand and characterize the mouth’s cells to gain insight into relevant diseases.
The Oral Mucosa
There are multiple types of cells making up the complex and dynamic structure of the oral mucosa and playing crucial roles in maintaining the health and functionality of the oral cavity. The oral mucosa is a tissue comprising several layers, each of which is with distinct cell types performing specific and essential functions for oral health. Scientists have known that the oral mucosa is mainly composed of four types of cells including epithelial cells from the surface layer of the oral mucosa, endothelial cells from the blood vessels that supply nutrition and oxygen, stromal cells which give structure to the mucosa, and immune cells that survey the surroundings to capture and destroy foreign particles.
This scientific article provides insight into the oral cell system by first introducing the basic cell types of the oral mucosa, especially several key cell types including oral epithelial cells (keratinized and non-keratinized epithelial cells), junctional epithelial cells, and fibroblasts. It is then followed by an in-depth introduction to oral squamous cell carcinoma (OSCC) which is closely related to epithelial cells of the oral mucosa, and its pathogenesis, clinical features, diagnosis, treatment, and applications.
Keratinized and Non-keratinized Epithelial Cells
When examining an individual oral cavity, the first and most prominent cell type being noticed is the oral epithelial cells since they are the primary cell type lining the oral cavity. Epithelium tissue is one of the four types of vital body tissue found in your organs and forms a thin protective layer acting as the first barrier against environmental factors, pathogens, and mechanical stress. In the oral cavity, these epithelial cells can be categorized into keratinized and non-keratinized epithelial cells, serving distinct functions due to their different biological characteristics.
Keratinized Epithelial Cells
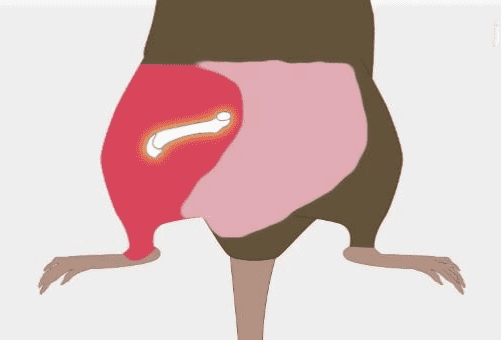
In general, the keratinized squamous epithelial cells form the stratum corneum, the outermost layer of the human epidermis (skin). These keratinized cells are called corneocytes, which are strong, dead keratinocytes that protect us from harm, including abrasions, pathogens, heat and light. This layer also consists of fats, keeping water from easily entering or leaving your body. The corneocytes consistently shed as new keratinocytes develop in the basal layer and move through the other layers of skin. The keratinized squamous epithelial cells are found in some very well-defined sites within the oral cavity, which undergo very severe mechanical stress. This includes the hard palate, the gingiva, and the dorsal of the tongue. In addition, there is a specialized mucosa on the dorsum of the tongue includes a number of papillae and is covered by a stratified squamous epithelium which can be either keratinized or non-keratinized [1]. Figure 1 shows the skematic of the cell layers of keratinized epithelium [2]. The keratinocytes throughout these layers actively produce keratin, a strong fibrous protein that anchors the cell together, and lipids both of which are essential for forming the epidermal water barrier. Moreover, as keratin is so strong, it won’t dissolve in diluted acids, alkalines, or solvents. Together, the keratinized epithelial cells are responsible for maintaining the barrier function and providing more effective protection of the oral mucosa including durability and resistance to mechanical abrasion, and they are crucial for areas exposed to friction from chewing.
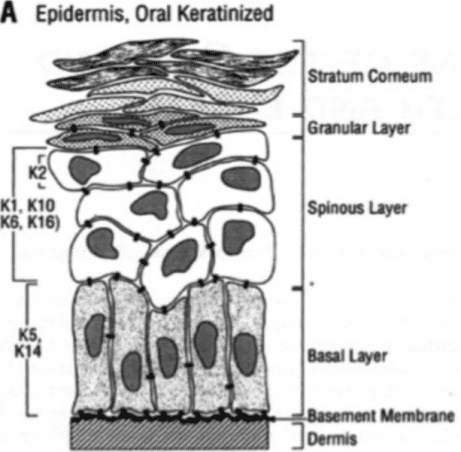
Figure 1. A schematic of the cell layers of keratinized epithelium.
Non-Keratinized Epithelial Cells
On the other hand, the non-keratinized epithelium is made up of the stratified squamous epithelial cells that lack the keratin protein. A schematic of the cell layers of non-keratinized epithelium is shown in Figure 2 [2]. These cells are the primary constituent of the oral mucosa, forming a protective layer on the inner surface of the oral cavity. They are commonly located on regions such as the inner lips, cheeks, ventral surface of the tongue, some sites on the gingiva, and floor of the mouth. In contrast to the keratinized epithelial cells, non-keratinized epithelial cells are moist and permeable to water, thus forms a less effective barrier [3]. Nevertheless, the moist environment maintained by the oral system is essential for many physiological activities. For one thing, the absence of keratin makes this tissue a wet, porous surface, which is essential for lubrication and protection. For another, it also makes the tissue more flexible and softer which is extremely necessary to bring elasticity and mobility for certain regions to facilitate movements such as speaking, chewing and facial expressions.
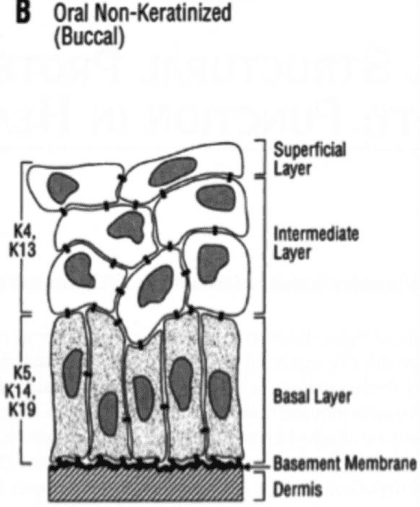
Figure 2. A schematic of the cell layers of non-keratinized epithelium.
Junctional Epithelial Cells
The gingiva, or gum tissue, is a specialized epithelial tissue that surrounds the structure of the teeth through a type of specialized cell known as junctional epithelial (JE) cells. This type of oral cell is derived from odontogenic epithelial cells right after the eruption. Nowadays, scientists believe that the JE cells are gradually being replaced by oral gingival epithelial cells which constitute the first barrier of periodontal tissue, and play an important role in resisting the invasion of periodontitis bacteria over the lifetime [4].
Fibroblasts
Fibroblasts are the most common type of stromal cells found abundantly in the connective tissues. Usually, they are believed to be mere producers of connective tissues, as they are well known for secreting proteins that constitute the extracellular matrix and playing an essential role in wound repair, tissue development, and fibrosis. In oral cavity, they are also an important type of cell in the oral and gingival tissues, playing crucial roles in the maintenance and repair processes of periodontal tissues. Recently, they became more attractive and caught scientists’ eyes thanks to a striking discovery of fibroblasts in the oral environment which unraveled their prominent immune signature particularly through recruiting neutrophils [5].
Oral Squamous Cell Carcinoma
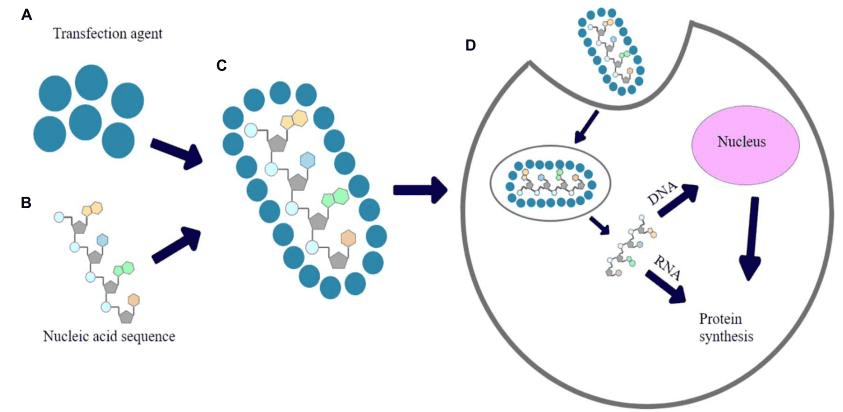
The oral squamous cell carcinoma (OSCC), a prevalent form of cancer originating from the squamous epithelial cells of the oral mucosa as introduced earlier, accounts for approximately 90% of oral malignancies and impairs appearance, pronunciation, swallowing and flavor perception [6]. It is considered to be one of the most common head and neck cancers, which has not shown any significant improvement over decades. The development of OSCC proceeds in a multistep fashion, which, more often than not, transpires over a long period. This multistep process in the development of OSCC, as in other human cancer ailments, is both environmentally influenced through lifestyle choices such as the use of tobacco and alcohol, as well as genetically dictated by the introduction of dysregulations in cellular pathways due to genetic mutations. Other risk factors such as betel quid (BQ) and human papillomavirus (HPV), often lead to the development of oral mucosal lesions known as oral potentially malignant disorders (OPMDs), which causes an increased risk of developing into OSCC [6, 7]. The consequences of uncontrolled cell proliferation would cause invasion of the surrounding tissues, which eventually end up in metastasis to distant organs through lymphatic outflow during the later phases. According to the Global Cancer Observatory in 2020, the annual cases of OSCC were 377,713 worldwide, the incidence will rise by approximately 40% by 2040, accompanied by a growth in mortality. Therefore, it is critical to understand the mechanisms of malignancies to facilitate the development of effective prevention, diagnosis, and treatment strategies.
The clinical features of OSCC depend on the site of the lesions. As shown in Figure 3, most of the OSCC lesions were detected at the posterior lateral border of the tongue [6]. Typically, OSCC appears as a non-healing ulcer with a white or red patch in the oral cavity. With the progression of the disease, more advanced ulceration develops with an uneven floor and distinct edges. The presence of ulceration is a sign that the disease is in the early stage and is typically painless. Early detection, just like in other types of cancer, is very crucial for the treatment of the disease. For instance, scientists recently discovered metabolic biomarkers that can aid in the early diagnosis of OSCC by analyzing metabolic changes in OSCC cells. These biomarkers might be crucial for developing precise diagnostic tools and tailored therapeutic strategies [8].
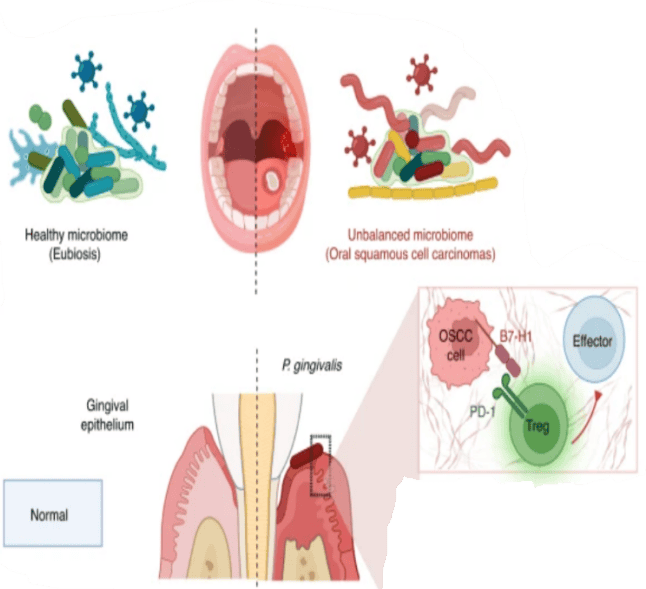
Figure 3. A typical OSCC of the tongue with morphological characteristics of ulceration.
Over all, the survival and prognosis of a OSCC patient definitely depend upon the evaluation of the progression and development of the disease in terms of angiogenesis, tumor budding, perineural invasion, staging, the presence of specific biomarkers, and HPV status, as these are all factors help to guide treatment decisions and assess the mortality rate of OSCC patients.
The cornerstone of OSCC treatment used to be surgical excision, often combined with radiotherapy or chemoradiotherapy [9]. Today, research into treatments for OSCC is also a direction that scientists are working toward, with more clinical solutions being promoted. For example, scientists have recently endorsed different types of immunotherapies such as tumor-infiltrating lymphocytes (TILs) in the early treatment of OSCC. Furthermore, research on OSCC has also employed artiffcial intelligence (AI) as a promising tool to analyze patient survival based on factors including staging and grading [10]. These emerging areas on the aspects of OSCC treatment further cement the multidisciplinary approach and technological advances in tackling this challenging disease.
Conclusions
The oral cell system includes many different cell types: epithelial cells, endothelial cells, stromal cells such as fibroblasts, and immune cells that are important for maintaining oral health and functions. OSCC, derived mainly from the squamous epithelial cells lining the oral cavity, is known to be a clinical challenge by its aggressiveness and intricate pathogenic process. The field of OSCC offers enormous potential for future research and treatment development, which could change the nature of early detection and personalized therapies and the development of new treatment modalities. Further areas of advancement would be through interdisciplinary efforts [8, 10].
| Cat. No | Product Name | Cell Type | |
|---|---|---|---|
| ABC-TC3733 | Human Oral Keratinocytes | Primary Cell Products | +inquiry |
| ABC-TC4365 | Human Oral Epithelial Cells | Primary Cell Products | +inquiry |
| ABC-TC134L | Human Gingival Epithelial Cells | Primary Cell Products | +inquiry |
| ABC-TC018W | Human Oral Fibroblasts | Primary Cell Products | +inquiry |
| ABC-TC3627 | Human Gingival Fibroblasts | Primary Cell Products | +inquiry |
| ABC-TC0419 | HSC-2 | Human OSCC Cell Lines | +inquiry |
| ABL-TC0290 | HSC-3 | Human OSCC Cell Lines | +inquiry |
| ABL-TC0112 | Ca9-22 | Human OSCC Cell Lines | +inquiry |
| ABL-TC0611 | SAS | Human OSCC Cell Lines | +inquiry |
| ABL-TC0617 | SCC-4 | Human OSCC Cell Lines | +inquiry |
References
[1] S. Groeger, J. Meyle, Oral mucosal epithelial cells, Frontiers in immunology 10 (2019) 208.
[2] S. Shetty, S. Gokul, Keratinization and its disorders, Oman medical journal 27(5) (2012) 348.
[3] C. Squier, The permeability of oral mucosa, Critical Reviews in Oral Biology & Medicine 2(1) (1991) 13-32.
[4] M. Kato, J. Tanaka, R. Aizawa, S. Yajima-Himuro, T. Seki, K. Tanaka, A. Yamada, M. Ogawa, R. Kamijo, T. Tsuji, Visualization of junctional epithelial cell replacement by oral gingival epithelial cells over a life time and after gingivectomy, Scientific Reports 9(1) (2019) 7640.
[5] D.W. Williams, T. Greenwell-Wild, L. Brenchley, N. Dutzan, A. Overmiller, A.P. Sawaya, S. Webb, D. Martin, G. Hajishengallis, K. Divaris, Human oral mucosa cell atlas reveals a stromal-neutrophil axis regulating tissue immunity, Cell 184(15) (2021) 4090-4104. e15.
[6] Y. Tan, Z. Wang, M. Xu, B. Li, Z. Huang, S. Qin, E.C. Nice, J. Tang, C. Huang, Oral squamous cell carcinomas: state of the field and emerging directions, International journal of oral science 15(1) (2023) 44.
[7] L. Lorini, C. Bescós Atín, S. Thavaraj, U. Müller-Richter, M. Alberola Ferranti, J. Pamias Romero, M. Sáez Barba, A. de Pablo García-Cuenca, I. Braña García, P. Bossi, Overview of oral potentially malignant disorders: from risk factors to specific therapies, Cancers 13(15) (2021) 3696.
[8] Y. Wang, X. Zhang, S. Wang, Z. Li, X. Hu, X. Yang, Y. Song, Y. Jing, Q. Hu, Y. Ni, Identification of metabolism-associated biomarkers for early and precise diagnosis of oral squamous cell carcinoma, Biomolecules 12(3) (2022) 400.
[9] P. Fiwek, N. Irga-Jaworska, S. Wojtylak, W. Biernat, K. Emerich, D. Pomiecko, Assessment of Cytological Changes in the Oral Mucosa in Young Hematological Patients Treated with Systemic Chemotherapy, Journal of Clinical Medicine 12(7) (2023) 2665.
[10] A. Almangush, A.A. Mäkitie, A. Triantafyllou, R. de Bree, P. Strojan, A. Rinaldo, J.C. Hernandez-Prera, C. Suárez, L.P. Kowalski, A. Ferlito, Staging and grading of oral squamous cell carcinoma: An update, Oral oncology 107 (2020) 104799.

Copyright - Unless otherwise stated all contents of this website are AcceGen™ All Rights Reserved – Full details of the use of materials on this site please refer to AcceGen Editorial Policy – Guest Posts are welcome, by submitting a guest post to AcceGen you are agree to the AcceGen Guest Post Agreement – Any concerns please contact [email protected]