- In-Stock Tumor Cell Lines
- Human Orbital Fibroblasts
- Human Microglia
- Human Pulmonary Alveolar Epithelial Cells
- Human Colonic Fibroblasts
- Human Type II Alveolar Epithelial Cells
- Human Valvular Interstitial Cells
- Human Thyroid Epithelial Cells
- C57BL/6 Mouse Dermal Fibroblasts
- Human Alveolar Macrophages
- Human Dermal Fibroblasts, Adult
- Human Lung Fibroblasts, Adult
- Human Retinal Muller Cells
- Human Articular Chondrocytes
- Human Retinal Pigment Epithelial Cells
- Human Pancreatic Islets of Langerhans Cells
- Human Kidney Podocyte Cells
- Human Renal Proximal Tubule Cells
Liver diseases are one of the most focused areas of clinical therapy and basic research. As the first immune cells in the liver, Kupffer cells show a critical role in the physiological and pathological processes of the liver. Therefore, Kupffer cells have become a research hotspot in liver diseases and a potential target for clinical treatment.
What are Kupffer Cells?
Kupffer cells are immune cells localized in the liver and conglutinate to vascular endothelium. And it is also known as Stellate Macrophages or Kupffer–Browicz cells. Kupffer cells were first observed in 1876 by Karl Wilhelm von Kupffer and identified as microphages in 1898 by Tadeusz Browicz[1].
The development of the cells begins in the yolk sac and migrates to the fetal liver. Eventually, the cells proliferate and differentiate into Kupffer cells in the end stage of embryonic development. The average life span of Kupffer cells is about 3.8 days, but it can be more than a year in rats and transplanted human livers[1, 2].
The shape of Kupffer cells is like an amoeboid. Microvilli, pseudopodia and lamellipodia exist on the cell surface and extend in all directions. The centrilobular and periportal regions of the liver are the distribution areas of Kupffer cells. And the structure of the cells will vary depending on their locations[1]. (Figure 1)
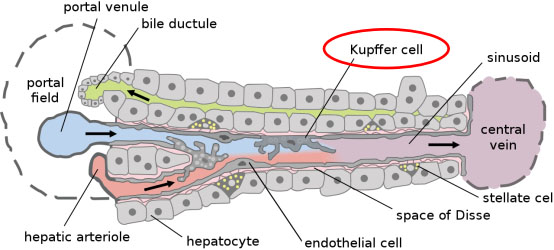
Figure.1 Kupffer cells in the liver infrastructure[1].
Physiological and Pathological Function of Kupffer Cells
Kupffer cells adhesive to the endothelial cells are the first immune cells in the liver. Therefore, Kupffer cells play a role in various liver diseases, including Alcoholic Liver Disease (ALD), hepatitis, liver fibrosis, etc.[1] And it plays a key role in maintaining liver homeostasis and the physiological activities of the whole body. The main functions of Kupffer cells include removing cell debris and metabolic waste, maintaining iron homeostasis, regulating cholesterol metabolism, mediating antibacterial defense, and promoting immune tolerance[3]. Besides, Kupffer cells are a part of the reticuloendothelial system in the liver. And it is also one of the maintainers of the liver tissue structure homeostasis[4].
Kupffer Cells Culture
The protocol of recovering and culturing Kupffer cells is similar to the primary cells, but the details are different. And Kupffer cells can be monocultures or co-cultured with Hepatocytes. The protocol refers to the technical documentation of thermofisher scientific.
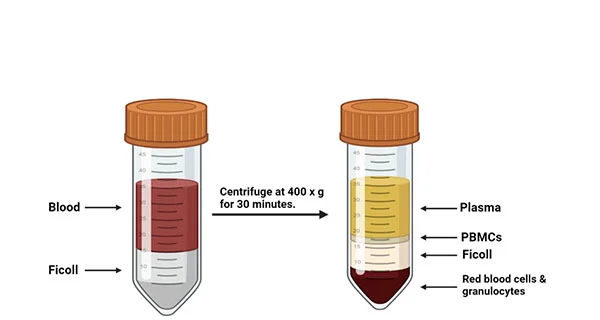
Take cell recovery in monoculture of Kupffer cells as an example. After thawing quickly in a 37°C water bath, dilute ten times with cold (4°C) medium (based on RPMI 1640) and place on ice (Kupffer cells are very viscous in 37°C medium). Centrifuge to isolate the cells at 500 × g for 5 min, resuspend in 1~2 mL medium, and counting the cells. And then, the cells can be plated into the plate coated with the substrate (collagen) and attach about 4~6 hours. After attachment for 4-6 hours, replace with fresh medium and incubate for 24 hours, and then the cells are ready for experiments.
If you want to co-culture Kupffer cells with Hepatocytes, you have to use the medium based on Advanced DMEM in the Kupffer cells recovery and culture. You can plate hepatocytes 4~48 hours after plating Kupffer cells, but the best recommendation is 24 hours.
Applications of Kupffer Cells
Kupffer cells are one of the key immune cells in the liver. The research methods used in the research of mechanisms of Kupffer cells in liver diseases include clinical trials, mouse models, rat models, and in vitro immortalized cell lines. Kupffer cells from different sources cultured in vitro have become a widely used in vitro experimental model.
– Application of Human Kupffer Cells in the Research of Liver Cirrhosis
Liver cirrhosis is a progressive syndrome. The main characteristics of liver cirrhosis include diffuse fibrosis, portal hypertension, etc. Acutely decompensated cirrhosis (AD) is a type of liver cirrhosis, and its clinical manifestations include jaundice, ascites, variceal bleeding, etc. Kupffer cells can express cytokines such as interleukin 35 (IL-35) to induce the expansion of suppressor CD4+ T cells, ending up with immuneparesis, which is one of the hallmarks of AD.
Khamri Wafa, et al. have identified the expansion of suppressor CD4+ T cells with the high expression level of human leucocyte antigen G (HLA-G) [5]. And the expansion of this particular subpopulation is mediated by IL-35. They performed immunohistochemistry staining on clinical samples of AD patients and identified the high expression of IL-35 in the distribution area of Kupffer cells. Then, they found a high expression level of IL-35 induced by Lipopolysaccharide (LPS) in Human Kupffer cells cultured in vitro. (Figure 2) These findings indicate the potential role of Kupffer cells in the pathology of liver cirrhosis.
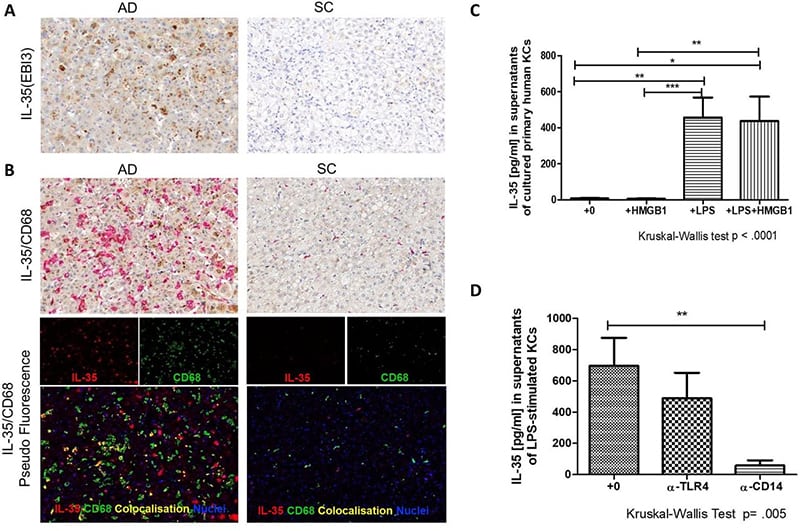
Figure 2. Kupffer cells are one of the cellular sources of IL-35 in liver cirrhosis[5].
– Application of Mouse Kupffer Cells in the Research of Liver Fibrosis
Momen-Heravi, et al. found that Kupffer cells are involved in microRNA-132 (miR-132)-induced liver fibrosis[6]. The inhibition of miR-132 by locked nucleic acid-anti-miR-132 can inhibit CCl4-induced liver fibrosis. While Matrix metalloproteases-12 (MMP-12) has the function of preventing liver fibrosis. Kupffer cells and hepatocytes were isolated from the mouse model and found that the inhibition of miR-132 level can induce MMP-12 level mainly in Kupffer cells. This publication shows the application of mouse primary Kupffer cells in the research of liver fibrosis.
Immortalized Mouse Kupffer cells (IMKCs) are also a valuable tool for researchers. For example, a research of the anti-inflammation effect of a polyphenol called catechin-7,4′-O-digallate (CDG) published by Kim, et al[7]. They treated IMKC with CDG and LPS and found that CDG can inhibit the expression of inducible nitric oxide synthase (iNOS) in IMKC and mediate the expression of some pro-inflammatory cytokines. And then, they identified CDG can inhibit the phosphorylation and degradation of IκBα and the activation of AT-rich interaction domain 5A (Arid5a) in the LPS-treated IMKC. These discoveries show that CDG can inhibit inflammation by inhibiting the NF-κB signal and Arid5a in the IMKC.
– Application of Rat Kupffer Cells in the Research of Liver Inflammation and Fibrosis
In a report about liver fibrosis and inflammation in rats, Liu, et al. found the activation and apoptotic of Kupffer cells in the rats’ liver fibrosis model[8]. And they identified that activated Kupffer cells can induce the activation of hepatic stellate cells (HSCs) through TNF-α in the CCl4-induced rats liver fibrosis model. Besides, they found that the collagen produced by Kupffer cells may play a role in the process of liver fibrosis. These findings show that Kupffer cells can be activated by drugs that induce liver damage and then promote the gradual deterioration of the liver disease. Therefore, Kupffer cells can be identified as a potential therapeutic target for liver disease.
Conclusion
Kupffer cells are important immune cells in the liver. It plays a key role in various physiological and pathological processes (such as liver fibrosis, liver inflammation, immuneparesis, etc.) in the liver and even the whole body. And Kupffer cells as a potential therapeutic target deserve more attention from researchers.
Where to Get Kupffer Cells for research?
Kupffer cells are invaluable tool for in vitro liver research. AcceGen provides different types of kupffer cells including Human Kupffer Cells, C57BL/6 Mouse Kupffer Cells, Immortalized Mouse Kupffer Cell Line (ImKC) and Rat Liver Kupffer Cells. It is our pleasure to help relative research to move forward. All the products of AcceGen are strictly comply with international standards. For more detailed information, please visit our product portfolio or contact inquiry@accegen.com.
Reference
1. wikipedia: https://en.wikipedia.org/wiki/Kupffer_cell.
2. Nguyen-Lefebvre AT, Horuzsko A: Kupffer Cell Metabolism and Function. J Enzymol Metab 2015, 1.
3. Wen Y, Lambrecht J, Ju C, Tacke F: Hepatic macrophages in liver homeostasis and diseases-diversity, plasticity and therapeutic opportunities. Cellular & Molecular Immunology 2021, 18:45-56.
4. Ju C, Tacke F: Hepatic macrophages in homeostasis and liver diseases: from pathogenesis to novel therapeutic strategies. Cellular & Molecular Immunology 2016, 13:316-327.
5. Khamri W, Gudd C, Liu T, Nathwani R, Krasniqi M, Azam S, Barbera T, Trovato FM, Possamai L, Triantafyllou E, et al: Suppressor CD4(+) T cells expressing HLA-G are expanded in the peripheral blood from patients with acute decompensation of cirrhosis. Gut 2021.
6. Momen-Heravi F, Catalano D, Talis A, Szabo G, Bala S: Protective effect of LNA-anti-miR-132 therapy on liver fibrosis in mice. Mol Ther Nucleic Acids 2021,
25:155-167.
7. Kim EJ, Seo JB, Yu JS, Lee S, Lim JS, Choi JU, Lee CM, Rashan L, Kim KH, Cho YC: Anti-Inflammatory Effects of a Polyphenol, Catechin-7,4′-O-Digallate, from Woodfordia uniflora by Regulating NF-κB Signaling Pathway in Mouse Macrophages. Pharmaceutics 2021, 13.
8. Liu C, Tao Q, Sun M, Wu JZ, Yang W, Jian P, Peng J, Hu Y, Liu C, Liu P: Kupffer cells are associated with apoptosis, inflammation and fibrotic effects in hepatic fibrosis in rats. Laboratory Investigation 2010, 90:1805-1816.

Copyright - Unless otherwise stated all contents of this website are AcceGen™ All Rights Reserved – Full details of the use of materials on this site please refer to AcceGen Editorial Policy – Guest Posts are welcome, by submitting a guest post to AcceGen you are agree to the AcceGen Guest Post Agreement – Any concerns please contact marketing@accegen.com