- Human Alveolar Macrophages
- BV-2
- Human Type II Alveolar Epithelial Cells
- Human Oral Keratinocytes
- Human Orbital Fibroblasts
- Human Intestinal Epithelial Cells
- Human Splenic Endothelial Cells
- Human NASH Peripheral Blood Mononuclear Cells
- MONO-MAC-6
- Human Adrenal Cortical Cells
- Human Pulmonary Alveolar Epithelial Cells
- Human Gastric Epithelial Cells
- Human Peripheral Blood Basophils
- Human Renal Interstitial Fibroblasts
- Human Astrocytes
- EBC-1
- MKN-1
- JIMT-1
why are hela cells special?
HeLa cells are special because they were the first human cells successfully cultured in vitro and can divide indefinitely in a laboratory environment, which makes them “immortal.” These cells were extracted in 1951 from a cervical cancer patient named Henrietta Lacks and have played a crucial role in many medical breakthroughs, including the development of the polio vaccine, cancer research, and gene mapping. Their ability to grow rapidly and continuously makes them a valuable tool in scientific research, although their use has raised important ethical issues regarding consent and ownership of biological materials.
Who is Henrietta Lacks?
Unlike the HeLa cell line that bears her name, little was known about Henrietta Lacks until the publication of Rebecca Skloot’s book, The Immortal Life of Henrietta Lacks, in 2010. Born in 1920 in Virginia, Henrietta was an African-American tobacco farmer, wife, and mother of five children. Henrietta was born in Virginia in 1920 and was an African American tobacco farmer, wife and mother of five children. In 1951, Henrietta died at the age of 31 from an aggressive form of cervical cancer, just 10 months after she first visited Johns Hopkins University seeking treatment for a “nodule” in her uterus. During her treatment at the hospital, a sample of cancerous tissue was removed from her cervix. These cells later became the immortalized cell line known as HeLa.
HeLa Cells: A Miracle of Scientific Research
HeLa cells are one of the most important cell lines in the history of science, widely recognized for their applications in medicine and biological research. These cells were derived from Henrietta Lacks, who sought treatment for cervical cancer at Johns Hopkins Hospital in 1951, and doctors extracted cells from her tumor. This marked the beginning of a remarkable journey, as these cells became the foundation for countless scientific studies.
1950s: The Origin and Early Applications of HeLa Cells
In 1951, Henrietta Lacks’s cells were named HeLa cells and quickly became the basis of medical research. In 1952, scientists successfully cultured these cells in the laboratory and published more than 110,000 research publications over the next 60 years. In 1953, researchers discovered that HeLa cells could effectively culture poliovirus, laying the foundation for the development of a polio vaccine.
1960s: Space Exploration and Blood Disease Research
In 1964, HeLa cells were sent into space, providing important data on how human cells respond to the space environment. In the same year, these cells were also used to study the potential therapeutic effects of hydroxyurea on blood cancers and sickle cell anemia, paving the way for future drug development.
1970s: Revealing the mechanism of bacterial infection
In 1973, scientists used HeLa cells to more rapidly study how salmonella causes infection. This discovery not only helped understand the pathogenic mechanisms of the bacteria, but also provided important information for the development of new diagnostics and treatments.
1980s: Major Breakthroughs in Cancer Research
In 1985, scientists discovered a link between human papillomavirus (HPV) and certain types of cervical cancer, laying the foundation for vaccine development. This research later won Dr. Harald zur Hausen a Nobel Prize in 2008. In addition, research on camptothecin has shown its potential in cancer treatment.
1990s: In-Depth Exploration of Disease Mechanisms
In 1993, HeLa cells were used to explore the molecular mechanisms of tuberculosis, providing valuable insights into the development of vaccines and treatments. Using these cells, researchers have gradually revealed the root causes of various diseases.
2000s: Technological Innovations and Major Discoveries
In 2001, researchers used HeLa cells to develop a novel single-cell imaging technique that allowed scientists to observe how viruses enter cells. This innovation laid the foundation for future Nobel Prize winners. In addition, research on HeLa cells revealed similarities between HIV and Ebola viruses, which helped vaccine research.
2010s: Progress in Ethics and Collaboration
In 2013, the National Institutes of Health reached an agreement with Henrietta Lacks’ descendants to allow them controlled access to the whole genome data of HeLa cells. This milestone reflects the U.S. government’s commitment to respecting the privacy of participants and the ethics of scientific research.
Conclusion
HeLa cells have not only played an important role in medical research, but also sparked important discussions about ethics and research practices. From their creation to the present, these cells have provided us with valuable insights into life, disease, and treatment, and have become an integral part of modern biomedical research. Henrietta Lacks’ story reminds us that scientific progress depends not only on technology and discovery, but also on a deep understanding and respect for human dignity and rights.
what are hela cells used for
HeLa cells have revolutionized medical science, contributing to six major breakthroughs: polio eradication, improved cell culture techniques, chromosome counting, the creation of genomic maps, the development of the HPV vaccine, and advancements in COVID-19 vaccines. These immortal cells continue to play a vital role in research and drug development.
1. Polio eradication
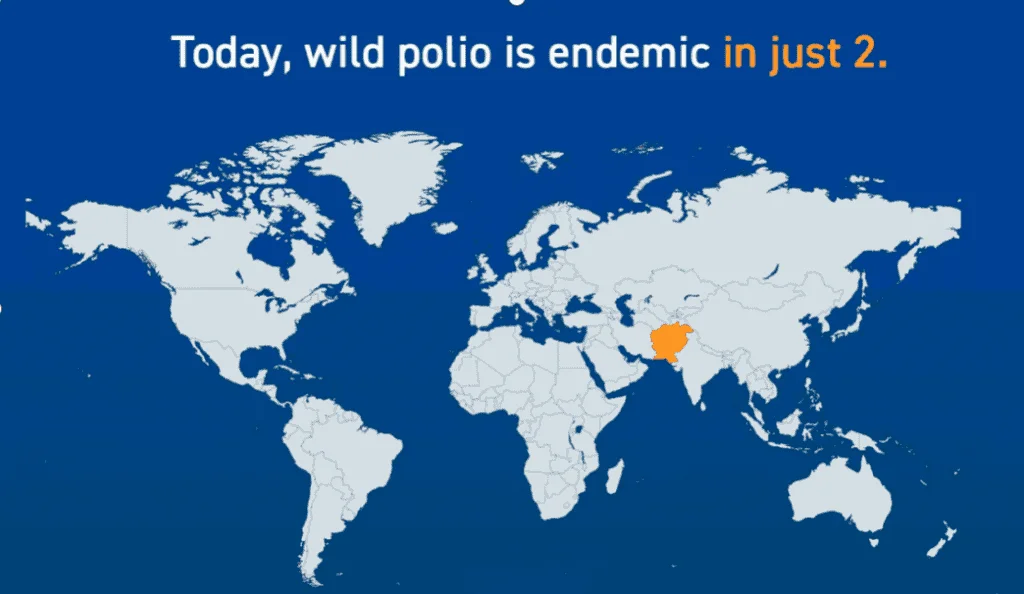
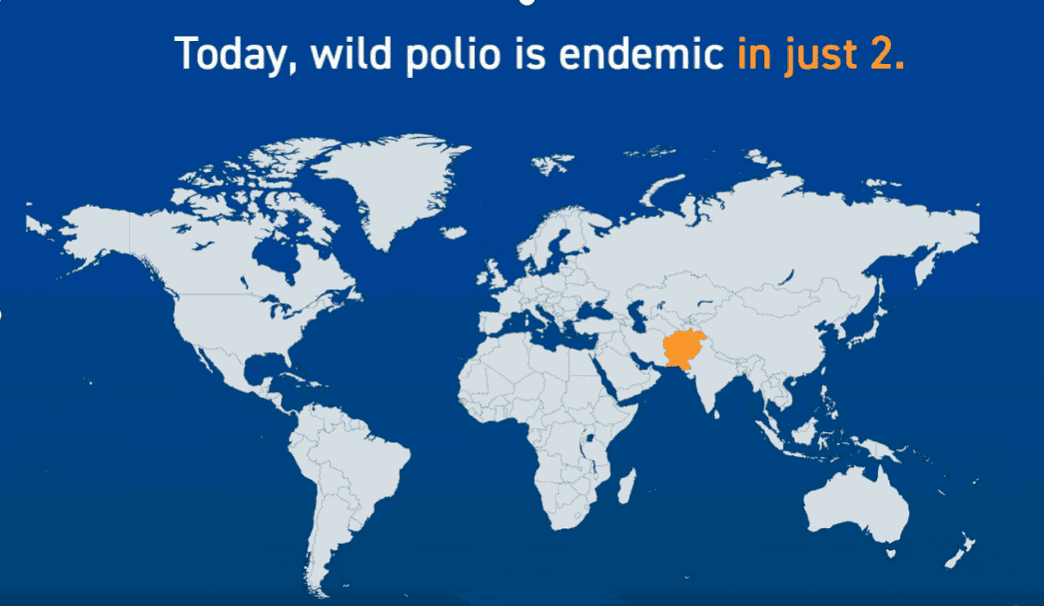
In the early 1950s, Jonas Salk developed a polio vaccine, but the high cost of conventional rhesus monkey cells made large-scale research difficult. In 1952, scientists discovered that HeLa cells could effectively infect polio but not be killed by the virus, making them ideal host cells. Tuskegee University established a HeLa cell culture laboratory that could provide about 20,000 test tube cultures per week at its peak. Since 1988, polio cases have dropped by more than 99%, from about 350,000 cases to only 6 cases reported in 2021.
1. Improving cell culture practices
When producing and distributing HeLa cells for polio vaccine testing at Tuskegee University at scale, principal investigators Brown and Henderson pioneered new cell culture protocols, including the use of rubber-lined screw-top vials and test tubes, as well as enhanced Quality control measures. Because HeLa cells are temperature sensitive, the researchers used multiple incubators and introduced new shipping solutions such as Equitherm and insulated shipping containers. After Gartler discovered that HeLa cells could become airborne and contaminate other cultures, cell culture practices improved significantly to prevent costly cross-contamination. More recently, HeLa cells have also been combined with artificial intelligence and machine learning to optimize culture media and further improve cell culture outcomes.
2. Chromosome count
In Rebecca Skloot’s book, The Immortality of Harrietta Lacks, she describes a 1953 laboratory error in Texas where researchers accidentally observed and counted every chromosome in HeLa cells. Based on this discovery, Tijo and Levan developed techniques to stain and count chromosomes chromosomes, confirming that human somatic cells have 23 pairs of chromosomes, not 24 as previously believed. This discovery is critical for medical diagnosis, as deviations from 23 pairs of chromosomes are associated with a variety of genetic disorders, such as trisomy 21 and Down syndrome.
3. Genome mapping
In 1965, Harris and Watkins created the first human-animal hybrid by fusing HeLa cells with mouse cells. Despite public fear and dismay at the time, this achievement fueled research into gene targeting of specific chromosomes and led to major advances in the Human Genome Project. These initial experiments culminated in the publication of the first complete human genome sequence in 2022. Today, genome mapping has led to multiple discoveries, such as how non-coding DNA mutations lead to many previously unexplained cases of neurodevelopmental disorders. In addition, genome mapping has been applied to stem cell research to understand potential differentiation trajectories and plays an important role in regenerative medicine.
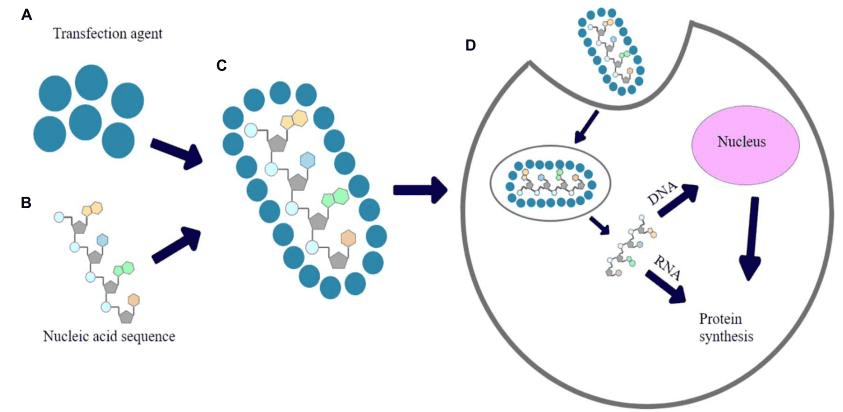
4. New Crown Vaccine
HeLa cells played a key role in identifying SARS-CoV-2 during the COVID-19 pandemic. Researchers used HeLa cells to identify the receptor used by the virus to infect host cells, a discovery that provided an important assistance in the initial identification of drugs and vaccines to treat and prevent infections. HeLa cells continued to play a role throughout the pandemic and were even used in the initial development of an mRNA vaccine against SARS-CoV-2.
Summarize
HeLa cells, derived from Henrietta Lacks, have transformed medical research since their introduction in the early 1950s, due to their unique ability to divide indefinitely. They have played a key role in the eradication of polio through the mass production of vaccines and have led to advances in cell culture practices that improve the reliability of research. HeLa cells have also contributed to important discoveries about the number of human chromosomes, aiding in the diagnosis of genetic diseases, and laid the foundation for the Human Genome Project, which has greatly advanced genetic research. Besides, they were instrumental in establishing the link between HPV and cervical cancer, leading to the development of effective vaccines, and played a key role in understanding SARS-CoV-2, aiding in the creation of vaccines during the COVID-19 pandemic. Beyond their scientific contributions, HeLa cells have sparked important ethical discussions regarding consent and the ownership of biological materials, reminding us that progress in medicine must be coupled with respect for individual dignity and rights.
Frequently asked questions about hela cells
Are hela cells still used
HeLa cells are still widely used in research due to their ability to divide indefinitely. Discovered in 1951, they have contributed to breakthroughs in cancer research, vaccine development, and cell biology. Despite early ethical concerns, they remain vital in modern science, with more than 110,000 studies relying on HeLa cells to make key medical advances.
are hela cells cancer cells
Yes, HeLa cells are cancer cells. They were originally taken from a cervical cancer tumor of Henrietta Lacks in 1951. These cells have the ability to divide uncontrollably, a key characteristic of cancer. Their rapid growth and ability to thrive in laboratory conditions make them “immortal” and valuable for scientific research.
what are the disadvantages of hela cells
HeLa cells have several disadvantages: they are genetically unstable, which can lead to inconsistent experimental results, and there is a risk of contaminating other cell cultures. Since HeLa cells are cancerous, they may not accurately represent normal healthy cells, limiting their applicability in certain studies. Additionally, their use continues to raise ethical concerns, as they were originally taken without consent.
References
[1] Scherer, W. F., Syverton, J. T., & Gey, G. O. (1953). STUDIES ON THE PROPAGATION IN VITRO OF POLIOMYELITIS VIRUSES. The Journal of Experimental Medicine, 97(5), 695–https://doi.org/10.1084/jem.97.5.695
[2] Puck, T. T., Marcus, P. I., & Cieciura, S. J. (1956). CLONAL GROWTH OF MAMMALIAN CELLS IN VITRO. The Journal of Experimental Medicine, 103(2), 273–https://doi.org/10.1084/jem.103.2.273
[3] Young, C. W., & Hodas, S. (1964). Hydroxyurea: inhibitory effect on DNA metabolism. Science, 146(3648), 1172–https://doi.org/10.1126/science.146.3648.1172
[4] Boshart, M., Gissmann, L., Ikenberg, H., Kleinheinz, A., Scheurlen, W., & Hausen, H. Z. (1984). A new type of papillomavirus DNA, its presence in genital cancer biopsies and in cell lines derived from cervical cancer. The EMBO Journal, 3(5), 1151–https://doi.org/10.1002/j.1460-2075.1984.tb01944.x
[5] Hsiang, Y. H., Hertzberg, R., Hecht, S., & Liu, L. F. (1985). Camptothecin induces protein-linked DNA breaks via mammalian DNA topoisomerase I. Journal of Biological Chemistry, 260(27), 14873–https://doi.org/10.1016/s0021-9258(17)38654-4
[6] Morin, G. B. (1989). The human telomere terminal transferase enzyme is a ribonucleoprotein that synthesizes TTAGGG repeats. Cell, 59(3), 521–https://doi.org/10.1016/0092-8674(89)90035-4
[7] Winners of the Nobel Prize in Physiology or Medicine. (n.d.). http://www.nobelprizes.org/nobel/medicine/
[8] Landry JJM, et al. Genes Genomes Genet. 2013
[9] The Immortal Life of Henrietta Lacks, the sequel. (n.d.). Center for Genetics and Society. https://www.geneticsandsociety.org/article/immortal-life-henrietta-lacks-sequel
[10] Lowrance, W. W., & Collins, F. S. (2007). Identifiability in genomic research. Science, 317(5838), 600–https://doi.org/10.1126/science.1147699

Copyright - Unless otherwise stated all contents of this website are AcceGen™ All Rights Reserved – Full details of the use of materials on this site please refer to AcceGen Editorial Policy – Guest Posts are welcome, by submitting a guest post to AcceGen you are agree to the AcceGen Guest Post Agreement – Any concerns please contact [email protected]