- In-Stock Tumor Cell Lines
- Human Orbital Fibroblasts
- Human Microglia
- Human Pulmonary Alveolar Epithelial Cells
- Human Colonic Fibroblasts
- Human Type II Alveolar Epithelial Cells
- Human Valvular Interstitial Cells
- Human Thyroid Epithelial Cells
- C57BL/6 Mouse Dermal Fibroblasts
- Human Alveolar Macrophages
- Human Dermal Fibroblasts, Adult
- Human Lung Fibroblasts, Adult
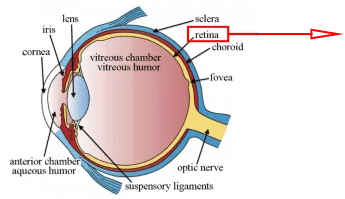
- Human Retinal Muller Cells
- Human Articular Chondrocytes
- Human Retinal Pigment Epithelial Cells
- Human Pancreatic Islets of Langerhans Cells
- Human Kidney Podocyte Cells
- Human Renal Proximal Tubule Cells
Endothelial cells (ECs) cover the lumen of blood vessels. Human umbilical vein endothelial cells (HUVECs) are a relatively simple and available human EC type, suitable for large scale preparation [1]. Thus, HUVECs are widely used in vitro model for ECs to study vascular endothelium properties and the main biological pathways involved in endothelium function.
Isolation and culture of HUVECs
The primary isolated Human Umbilical Vein Endothelial Cells are the most popular ECs used in a number of researches probably because human umbilical veins are relatively more available than other types of blood vessels. Generally, primary HUVECs need to be isolated from human umbilical vein vascular wall by a collagenase treatment, then inoculated on coated culture flask and incubated in a 37 °C-5% CO2 incubator by standard protocol with a relatively minimal equipment. Cell confluency can be monitored by phase-contrast microscopy [1]. Of course, the primary Human Umbilical Vein Endothelial Cells can also be directly purchased from commercial resources, e.g., AcceGen.
How to isolate HUVECs
Check whether the umbilical cord is suitable for use and treat the cord as follows:
- 1.
Tidily cut both ends of the cord with a scalpel.
- 2.
Insert a cannula at the end of each vein and secure them tightly with Nylon thread. Umbilical vein is the widest vessel and must not be confounded with the two arteries.
- 3.
Wash the vein with 100 mL PBS to remove traces of blood and drain the vessel.
- 4.
Perfuse the vein with 10 mL of 0.2% collagenase solution when the effluent buffer is transparent or slightly pink.
- 5.
Incubate the cord in a water bath at 37 °C for 15 minutes.
- 6.
Collect the cells in 50mL sterile test tubes containing 10 mL of Medium 199 (M-199) enriched with 20% fetal bovine serum (FBS) by flushing the vein with 30 mL PBS.
- 7.
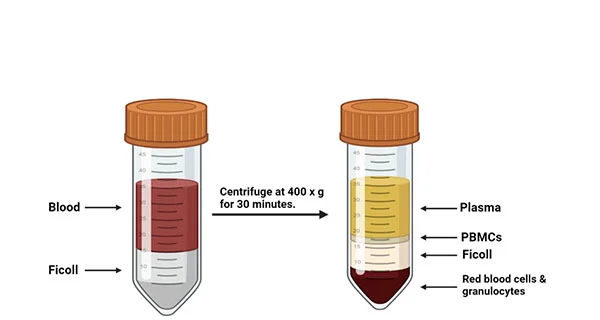
Centrifugate at 250 g for 10 minutes and wash with 20 mL of enriched M-199.
- 8.
Resuspend the pellet in 5 mL of fresh culture medium. The yield of this procedure is in the range of 0.5-1.5×106 cells per cord [1-3].
How to culture HUVECs
- 9.
Plate the 4 ml of medium with the cells (from step 8) in a 25-cm2 flask. Seeding conditions: 5-6 ×104 cells per 25 cm2 flask. To ensure cell attachment, the flasks should be coated with fibronectin or gelatin in advance.
- 10.
Incubate the flask in a 37ºC, 5% CO2/95% air, humidified cell culture incubator.
The reagents and conditions necessary for human umbilical vein endothelial cell culture are shown in Table 1. M199 is the most commonly used medium of human umbilical vein endothelial cells. Typically, the confluent primary cultures of HUVECs can be obtained in 6-8 days. Upon reaching 80-90% confluence, HUVECs can be used in subculture, obtained with or without trypsin treatment, for amplification of the number of cells.
Table 1 HUVECs culture conditions [2]

HUVEC Identification
It is well known that characteristics of the vascular endothelium are heterogeneity of morphological and functional aspects, cell activation marker proteins and response to growth factors. Jaffe first characterized the morphology of HUVECs in 1973 [2]. As shown in Figure 1, HUVECs possess a typical epithelioid morphology in a confluent monolayer, which is in a hexagonal or cuboidal form with long, round and slightly overlapping nuclei. There are different cell markers identified in the cytoplasm or ECs membrane. And HUVECs express many important endothelial markers, e.g., PECAM-1(CD31), ICAM-1(CD54), VCAM-1 (CD106) and selectins [1, 2]. Figure 2 demonstrates protein markers in HUVECs, and these protein markers can be identified in HUVECs by using antibodies. For example, PECAM-1(CD31) is a membrane glycoprotein found at endothelial intercellular junctions. The main function of this molecule is to regulate the EC-EC and EC-leukocyte adhesion. It can be identified by flow cytometry or by immunofluorescence.

Figure 1. Microscopy view of HUVEC (40X). The photomicrograph shows the morphological
characteristics of HUVEC. A confluent monolayer in a hexagonal or cuboidal form with large nuclei is observed [2].

Figure 2. Protein markers in HUVEC
HUVECs Model Applications
Various experimental models can be applied to reveal human physiological and pathological conditions. Compared to animal models, HUVECs models seems to better reflect some aspects of human diseases, such as cardiovascular and metabolic diseases.
HUVECs & Cardiovascular Diseases
Cardiovascular Diseases (CVD), including highly prevalent disorders such as hypertension, atherosclerosis, are highly prevalent in the adult population and the globally leading cause of death. CVD can affect the structure and function of the heart and blood vessels. And several metabolic risk factors which are involved in the development of CVD, such as hypercholesterolemia and diabetes, would promote EC dysfunction. Recently HUVEC model has been used to study pathophysiological mechanisms of CVD development.
Hypertension is a multifactorial chronic disease which can induce endothelial dysfunction by decreasing the secretion of NO and endothelin in EC, which leads to arterial vasoconstriction and favors apoptosis. Kriegel et al. demonstrated the higher microRNA-34a expression in peripheral blood of patients with hypertension than controls [4]. MicroRNA-34a inhibition in HUVEC boosted proliferation, migration, and G1-S transition of EC. Through bioinformatics, it is predicted that mRNA of the transforming growth factor β-induced factor homeobox 2 (Tgif2) is the target of microRNA34-a, indicating that microRNA-34a might be a potential diagnostic biomarker [5].
Atherosclerosis is a chronic inflammatory disease characterized by immune cells in the subendothelium and the accumulation of low-density lipoproteins (LDL), which can lead to the formation of an atherosclerotic plaque. Currently, Kisspeptin-10 (KP-10), a potent vasoconstrictor and inhibitor of angiogenesis, and its receptor GPR54 have drawn much attention with respect to atherosclerosis, as both KP-10 and GPR54 are highly expressed in atheromatous plaques and restenotic lesions after wire-injury. Takuya Watanabe et al. introduced the emerging roles of the KP-10/GPR54 system in atherosclerosis in their recent review paper [6]. It shows that KP -10 suppresses migration and proliferation of HUVECs, induces senescence in HUVECs and promotes adhesion of human monocytes to HUVECs. These findings implicate that KP -10 may contribute to acceleration of progression and to the instability of atheromatous plaques, resulting in rupture of plaques. This GPR54 antagonist can used to prevent and treat atherosclerosis. Therefore, the KP-10/GPR54 system may be a new therapeutic target for atherosclerotic diseases.
HUVEC Angiogenesis Assay
Angiogenesis is a complex physiological process which involves EC activation, migration, and proliferation which ends with the formation and organization of tubular structures to form new blood vessels [2]. HUVECs models have been used to research the molecular and signaling pathways of angiogenesis. According to Voellenkle et al., 400 microRNAs were identified and can be differentially expressed in HUVEC associated with angiogenesis under hypoxic conditions. The study suggests these microRNAs are potential biomarkers and therapeutic targets in ischemic heart disease [7]. Besides, HUVECs models have been applied to evaluate the pro-angiogenic effect of proteins (e.g., irisin) and drugs, such as Evolocumab, metformin, and cilostazol, which may provide additional therapeutic benefits in CVD [2].
In addition, angiogenesis is the underlying cause of many neoplastic diseases. It is also the basis of tumor metastasis. Abdul Qadir et al. used Human Umbilical Vein Endothelial Cells as an in vitro model to determine the synergistic effect of drugs, such as bevacizumab and celecoxib, on angiogenesis [8]. Their results demonstrate that bevacizumab and celecoxib have a synergistic effect in inhibiting in vitro angiogenesis and their combination contributed stronger inhibition than either drug alone.
Nanotoxicological and nanomeidicine study
In nanotoxicological and nanomedicine studies, ECs are attracting particular interests according to the following two reasons. One the one hand, ECs are the first contact for nanoparticles (NPs) entering the blood before being delivered to targets. On the other hand, ECs play a critical role in regulating blood vessel tone, homeostasis, and hormone transport, and dysfunction of ECs has been implicated in the development of CVDs. Thus, the assessment of the toxicity of NPs to ECs may offer important information about the side effects of NPs. HUVECs, served as a simple and relatively reliable in vitro model for ECs, could asses and predict the toxicity of NPs to endothelium.
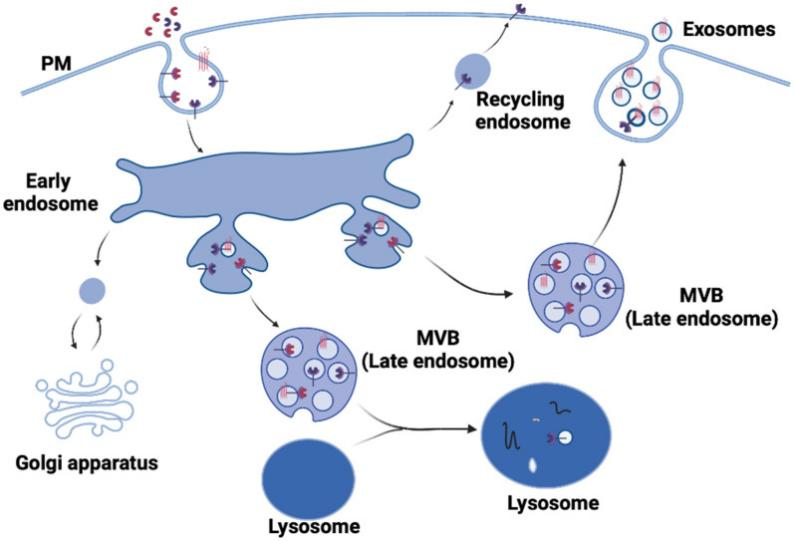
Cao Yi et al. reviewed that in some studies, HUVECs have been used as a model to investigate the ECs-NPs interactions, the toxic effects of NPs on ECs and the relevant mechanisms. The results of these studies indicated that NPs could be internalized into HUVECs through the endocytosis pathway and can be transported across HUVECs by exocytosis and paracellular pathways. HUVECs exposure to NPs could lead to cytotoxicity, genotoxicity, eNOS uncoupling and endothelial activation, probably by NP-induced oxidative stress, inflammatory response and dysfunction of organelles. Moreover, some studies also assessed the effects of microenvironment (e.g. the presence of proteins and excessive nutrients), the physiological and pathological stimuli related to the diversity of ECs (e.g. shear stress, cyclic stretch and inflammatory stimuli) [9].
Conclusions
There have been many exciting developments in isolation, culture, characterization and application of Human Umbilical Vein Endothelial Cells. HUVECs serve as an excellent in vitro model to study the endothelium and have also provide facilities and benefits, particularly for researches on such diseases as cardiovascular and metabolic diseases.
Where to Get Human Umbilical Vein Endothelial Cells?
HUVECs are the best-characterized endothelial cells and can be easily isolated and cultured in a laboratory setting. AcceGen provides a series of human umbilical vein cells for specific research needs. The detailed product list is as follows.
All the products of AcceGen are strictly comply with international standards. For more detailed information, please visit our product portfolio or contact [email protected].
Reference
1. Bruno Baudin, Arnaud Bruneel, Nelly Bosselut & Michel Vaubourdolle: A protocol for isolation and culture of human umbilical vein endothelial cells. Nature Protocols 2007(2): 481–485.
2. Diana J. Medina-Leyte, Mayra Domínguez-Pérez, Ingrid Mercado, María T. Villarreal-Molina, et al: Use of Human Umbilical Vein Endothelial Cells (HUVEC) as a Model to Study Cardiovascular Disease: A Review. Appl. Sci. 2020(10) 3: 938-962
3. Commonly used methods for cell culture (b): Isolation and culture of human umbilical vein endothelial cells. 2007.
4. Kriegel A.J., Baker M.A. Liu Y., Liu P., et al: Endogenous microRNAs in human
microvascular endothelial cells regulate mRNAs encoded by hypertension-related genes. Hypertension 2015 (66):793–799.
5. Liu S.G., Yi F.F., Cheng W.W., Qu X., et al: Molecular mechanisms in vascular injury induced by hypertension: Expression and role of microRNA-34a. Exp. Ther. Med. 2017(14):5497–5502.
6. Takuya Watanabe, Kengo Sato: Roles of the kisspeptin/GPR54 system in pathomechanisms of atherosclerosis. Nutr Metab Cardiovasc Dis. 2020, 30(6):889-895.
7. Voellenkle C., Rooij J., Guffanti A., Brini E., et al: Deep-sequencing of endothelial cells exposed to hypoxia reveals the complexity of known and novel microRNAs. RNA 2012(18):472–484.
8. Abdul Qadir, Mohsin Wahid, Mahayrookh Asif, Talat Roome: Synergistic effect of bevacizumab and celecoxib on angiogenesis in vitro using human umbilical vein endothelial cells. Int J Clin Pharmacol Ther. 2020, 58(12):696-702.
9. Yi Cao, Yu Gong, Liangliang Liu, Yiwei Zhou, et al: The use of human umbilical vein endothelial cells (HUVECs) as an in vitro model to assess the toxicity of nanoparticles to endothelium: a review. J Appl Toxicol. 2017, 37(12):1359-1369.

Copyright - Unless otherwise stated all contents of this website are AcceGen™ All Rights Reserved – Full details of the use of materials on this site please refer to AcceGen Editorial Policy – Guest Posts are welcome, by submitting a guest post to AcceGen you are agree to the AcceGen Guest Post Agreement – Any concerns please contact [email protected]