- In-Stock Tumor Cell Lines
- Human Orbital Fibroblasts
- Human Microglia
- Human Pulmonary Alveolar Epithelial Cells
- Human Colonic Fibroblasts
- Human Type II Alveolar Epithelial Cells
- Human Valvular Interstitial Cells
- Human Thyroid Epithelial Cells
- C57BL/6 Mouse Dermal Fibroblasts
- Human Alveolar Macrophages
- Human Dermal Fibroblasts, Adult
- Human Lung Fibroblasts, Adult
- Human Retinal Muller Cells
- Human Articular Chondrocytes
- Human Retinal Pigment Epithelial Cells
- Human Pancreatic Islets of Langerhans Cells
- Human Kidney Podocyte Cells
- Human Renal Proximal Tubule Cells
Introduction: Retina and Retinal Pigment Epithelium
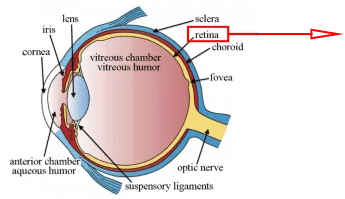
Retina is a light-sensitive tissue layer of the visual system, which is a part of the central nerve system. Its primary function is to transform incoming light signals into neural electrical signals and then transmit them to various visual centers in the brain to complete visual perception[1]. The vertebrate retina comprises 10 distinct layers, including the inner limiting membrane, nerve fiber layer, ganglion cell layer, inner plexiform layer, inner nuclear layer, outer plexiform layer, outer nuclear layer, external limiting membrane, inner/ outer segment layer, retinal pigment epithelium[2]. (Figure.1) These layers cover the entire process of the retina, from receiving light signals to converting them into neural signals and completing the transmission.
(a)
(b)
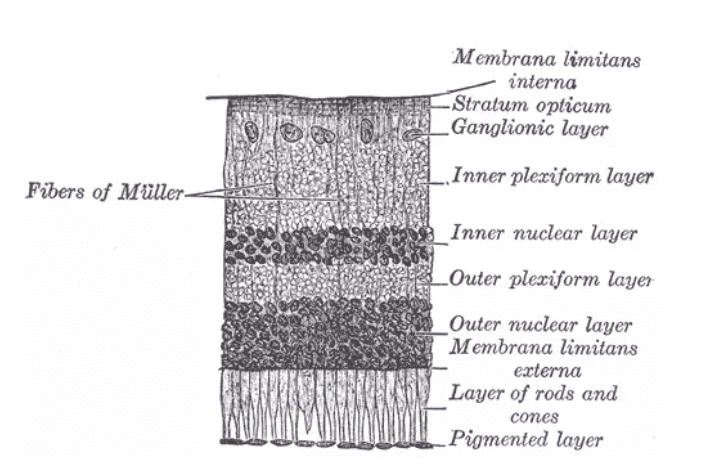
Figure.1 Eye and retina. (a) The physiological structure of the eyes[3]. (b) Biopsy slices of the retina[4].
Retinal pigment epithelium (RPE) is the part of the ten-layer structure of the retina , positioned farthest from the vitreous body, which is the pigmented cell layer just outside the neurosensory retina[5]. The functions of RPE can be summarized as light absorption, maintenance of retinal physiological and biochemical environment, blood-retinal barrier, and nutrient supply[6]. RPE contains black ferrite that can absorb scattered light to improve the quality of the optical system and diminish the photo-oxidative stress. As a maintainer of the retina, RPE acts as the blood-retinal barrier, the secretors of immune, energy, and signaling factors, nutrients transporters and providers. Additionally, RPE plays a crucial role in phagocytosis and clearance of phagocytosis of photoreceptor outer segment (POS) that has suffered damage and been detached due to photooxidative stress. The critical significance of RPE in maintaining retinal function underscores the potential gravity of pathological deviations in this stratum. For example, albinism leads to insufficient or missing retinal melanin, which possibly lead to visual dysfunction or even loss in patients[7]. Furthermore, macular degeneration and retinitis pigmentosa are the diseases related to pigments that impair light absorption and affect visual perception[8; 9]. Moreover, RPE is also involved in the pathological processes of diabetic retinopathy[10].
Human Retinal Pigment Epithelial Cells and Culture Protocol
Human source RPE in vitro models are indispensable for the research of physiology and pathology of retina and RPE. Primary human RPE cells (hRPECs) and immortalized cell lines are both used in the research. Immortalized cell lines are typically used to complete the majority of routine in vitro experiments, and ARPE-19 is one of the most widely used cell lines[11]. Primary cells are applied to high-value experiments and secondary validation of immortalized cell lines to enhance the credibility of research findings and conclusions, which are isolated from fresh clinical samples from the donors. Furthermore, iPSCs-induced differentiation is a pioneering pathway for obtaining RPE in vitro, including 3D culture, explants, organoids, and other emerging in vitro model technologies that are rapidly developing[12].
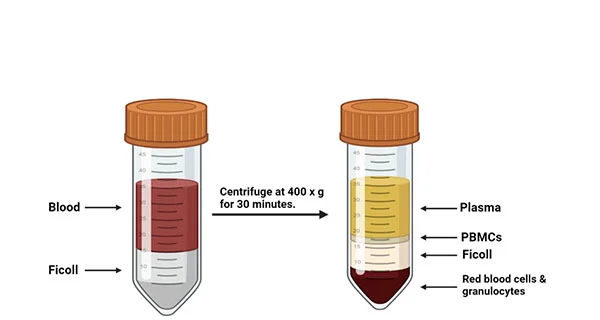
In this section, we give a brief introduction to culture methods and protocol for RPE immortalized cell lines (ARPE-19), and the isolation and culture protocol for primary hRPECs. The cells are cultured in DMEM/F12 medium with 10% FBS and 1% penicillin and streptomycin in 37℃, 5% CO2[13]. Primary hRPECs are isolated from fresh eye samples (within 24 hours of donor death). The eye is placed in 10cm2 plate filled with PBS, and all extraneous ocular tissues are meticulously removed. Subsequently, the entire neuroretina is meticulously extracted through anatomical dissection. The exposed RPE layer, distinguished by its dark brown single-layer appearance, is rinsed with PBS and then dissected into small fragments. The tissue is subsequently subjected to enzymatic digestion by dispase I solution in a culture environment (37℃, 5% CO2) for approximately 50 minutes, and then the hRPECs are isolated from the tissue suspension through centrifugation and subsequently cultured in the medium (DMEM/F10 with 12% FBS and other component)[14].
Application of Human Retinal Pigment Epithelial Cells in the Publications
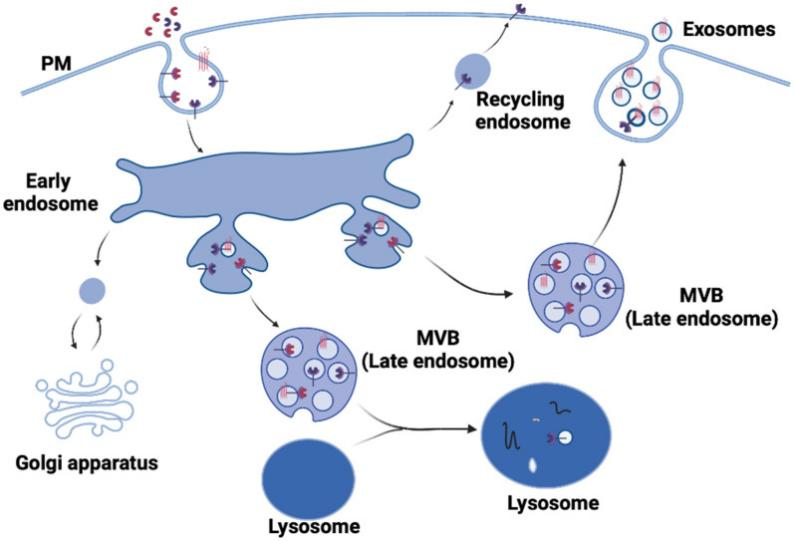
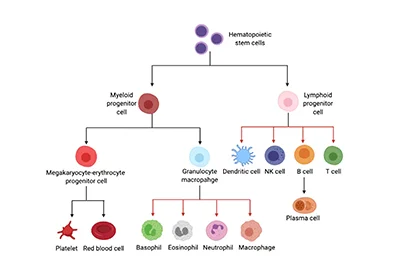
In vitro models employing human source RPE cells are used in the research of the diseases related to the retina and RPE, such as diabetic retinopathy (DR) and age-related macular degeneration. Based on human fetal RPECs and RPE-specific conditional knockout and knock-in mouse models, Liu et al. revealed the role of AKT in the pathological processes of DR and found a potential treatment method of DR through AKT[15]. They found that the activity of Akt1 and Akt2 regulated each other in DR, and the loss of Akt2 led to compensatory upregulation of phosphorylated Akt1 and then reduced diabetes-induced retinal abnormalities. In this process, the vascular injury, inflammatory cytokine release, and infiltration of immune cells mediated by the GSK3β/NF-κB signaling pathway were inhibited. These discoveries indicated that Akt1 in RPE was a potential target for the treatment of DR. In another publication, Lee et al. used human RPE cell lines ARPE-19 to identify a novel pathological mechanism in age-related macular degeneration[16]. They found that NMDA (N-methyl-D-aspartate) receptor antagonist induced the autophagy of ARPE-19 , leading to degradation of A2E (N-retinylidene-N-retinylethanolamine, a component of lipofuscin) in cells. This mechanism implies that NMDA receptor antagonist is a potential treatment method for the accumulation of lipofuscin in RPE in age-related macular degeneration.
Conclusion
RPE is one of the core parts of the retina, which is indispensable for maintaining human visual function and visual perception ability. Its pathological changes can range from mild to severe, leading to blindness. Therefore, the pathological research on retinal pigment epithelium is of great significance. Mastering the application methods of human retinal pigment epithelial cells, which are the most widely used in vitro models of RPE, is necessary.
Where to Get Nervous System Primary Cells for Your Research?
AcceGen isolates and offers a wide range of high-quality nervous system primary cells, such as Human Retinal Pigment Epithelial Cells, Human Oligodendrocyte Progenitor Cells, Human Microglia, and Human Schwann Cells. These cell products provide you with a convenient means to research. To get more information, please refer to: Nervous System Primary Cells.
It is our pleasure to help relative researches to move forward. All the products of AcceGen are strictly comply with international standards. For more detailed information, please visit our product portfolio or contact [email protected].
References
[1] W.J. Krause, Krause’s Essential Human Histology for Medical Students, Universal Publishers, 2005.
[2] The Retinal Tunic. Virginia–Maryland Regional College of Veterinary Medicine.
[3] wikipedia, and encyclopedia, Retina. https://encyclopedia.thefreedictionary.com/_/viewer.aspx?path=e%2Fe4%2F&name=120px-Three_Main_Layers_of_the_Eye.gif&url=https%3A%2F%2Fencyclopedia.thefreedictionary.com%2FRetina.
[4] wikipedia, and encyclopedia, Retina
[5] B. Cassin, and M.L. Rubin, Dictionary of Eye Terminology, Triad Publishing Company, 2001.
[6] S. O, The retinal pigment epithelium in visual function. Physiol Rev (2005).
[7] W.T. Allison, T.E. Hallows, T. Johnson, C.W. Hawryshyn, and D.M. Allen, Photic history modifies susceptibility to retinal damage in albino trout. Vis Neurosci 23 (2006) 25-34.
[8] R.S. Apte, Age-Related Macular Degeneration. New England Journal of Medicine 385 (2021) 539-547.
[9] K. Shintani, D.L. Shechtman, and A.S. Gurwood, Review and update: current treatment trends for patients with retinitis pigmentosa. Optometry 80 (2009) 384-401.
[10] D. Tonade, and T.S. Kern, Photoreceptor cells and RPE contribute to the development of diabetic retinopathy. Prog Retin Eye Res 83 (2021) 100919.
[11] L. Feng, L. Liang, S. Zhang, J. Yang, Y. Yue, and X. Zhang, HMGB1 downregulation in retinal pigment epithelial cells protects against diabetic retinopathy through the autophagy-lysosome pathway. Autophagy 18 (2022) 320-339.
[12] M.J. Song, R. Quinn, E. Nguyen, C. Hampton, R. Sharma, T.S. Park, C. Koster, T. Voss, C. Tristan, C. Weber, A. Singh, R. Dejene, D. Bose, Y.-C. Chen, P. Derr, K. Derr, S. Michael, F. Barone, G. Chen, M. Boehm, A. Maminishkis, I. Singec, M. Ferrer, and K. Bharti, Bioprinted 3D outer retina barrier uncovers RPE-dependent choroidal phenotype in advanced macular degeneration. Nature Methods 20 (2023) 149-161.
[13] R. Li, H. Li, and Q. Zhang, Procyanidin protects human retinal pigment epithelial cells from high glucose by inhibiting autophagy. Environmental Toxicology 37 (2022) 201-211.
[14] H. Shamsnajafabadi, Z.S. Soheili, S. Samiee, H. Ahmadieh, E.R. Pirmardan, and M. Haghighi, Neural differentiation of human retinal pigment epithelial cells on alginate/gelatin substrate. Mol Vis 28 (2022) 412-431.
[15] H. Liu, N.A. Stepicheva, S. Ghosh, P. Shang, O. Chowdhury, R.A. Daley, M. Yazdankhah, U. Gupta, S.L. Hose, M. Valapala, C.S. Fitting, A. Strizhakova, Y. Shan, D. Feenstra, J.A. Sahel, A. Jayagopal, J.T. Handa, J.S. Zigler, Jr., P.E. Fort, A. Sodhi, and D. Sinha, Reducing Akt2 in retinal pigment epithelial cells causes a compensatory increase in Akt1 and attenuates diabetic retinopathy. Nat Commun 13 (2022) 6045.
[16] J.R. Lee, and K.W. Jeong, NMDA Receptor Antagonists Degrade Lipofuscin via Autophagy in Human Retinal Pigment Epithelial Cells. Medicina (Kaunas) 58 (2022).


Copyright - Unless otherwise stated all contents of this website are AcceGen™ All Rights Reserved – Full details of the use of materials on this site please refer to AcceGen Editorial Policy – Guest Posts are welcome, by submitting a guest post to AcceGen you are agree to the AcceGen Guest Post Agreement – Any concerns please contact [email protected]